New Anthony Nolan research
New research from Anthony Nolan shows that identifying and addressing healthcare inequities remains an urgent priority in stem cell transplantation.
The work, in collaboration with the UK stem cell transplant organisation BSBMTCT, looked at historical UK transplant data from between 2009-2020, revealing there were differences in survival rates for patients from minority ethnic backgrounds receiving a stem cell transplant from a donor. It aimed to improve health services for future transplant patients.
On average, Black and Asian patients had worse survival rates compared to White patients following a stem cell transplant.
The study could not provide a reason for these inequities, but highlights that we must urgently do more work to understand healthcare inequity in stem cell transplants.
Dr Neema Mayor, Anthony Nolan’s director of immunogenetics and research services and lead author of the study, says:
Despite stem cell transplants having been used as a treatment for blood cancer and blood disorders for over 50 years, until now there was little known about the health inequalities experienced by patients in the UK. Our research shows for the first time that ethnicity affects survival following a stem cell transplant, with Asian and Black patients the most likely to die after transplant.
Our research is actively investigating these inequities, so we can continue to work to ensure all patients have equal access to, experience of and outcomes from a stem cell transplant.
Dr Neema Mayor, director of immunogenetics and research services, Anthony Nolan
The results
This is the first study on the impact of ethnicity on stem cell transplant in the UK.
It looked back at data from stem cell transplants in the NHS between 2009-2020, including 13,978 patients who received a transplant from a donor. Of these patients, 441 had described their ethnicity as “Black,” 1,081 as “Asian,” 751 as “Other” and 11,705 as “White.”
For this research, the level of tissue type matching between patients and donors was accounted for in the analysis. This means that any differences in survival were independent of matching status and other factors that we know can affect outcomes.
Overall, the study showed that patients of Asian, Black and Other ethnicities had worse survival than White patients at various timepoints after a transplant.
For cancer patients of any age undergoing a donor transplant, Black and Asian patients were 1.5 times more likely to die within five years of a donor transplant compared to White patients.
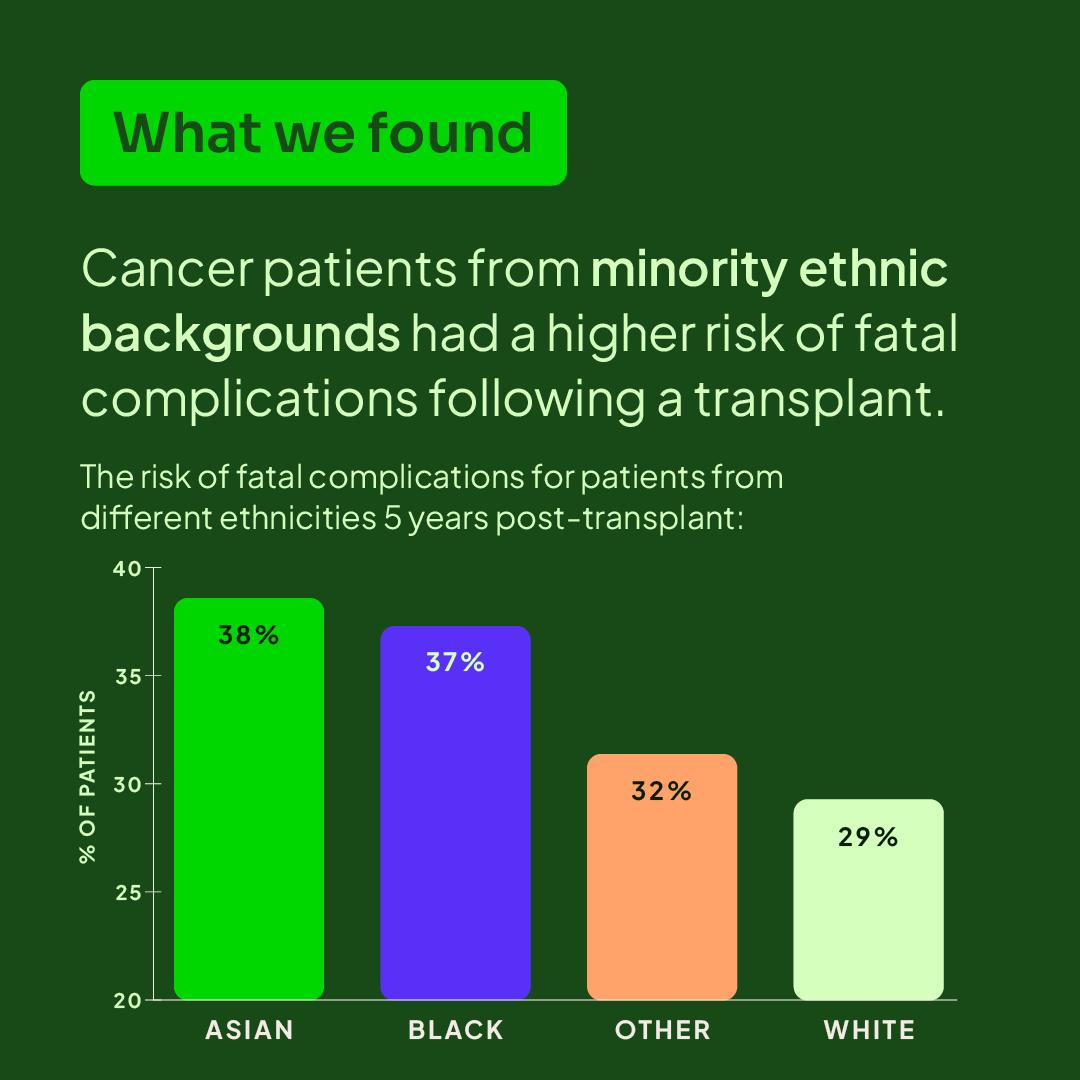
For paediatric cancer patients undergoing a donor transplant, Asian patients had the highest risk of fatal complications, with a 32% risk of death in the five years after a transplant, compared with 16% for Black patients, 15% for Other patients and 15% for White patients.
It’s important to remember that while these numbers might seem concerning, for most of these patients a stem cell transplant will be their best and often only treatment option for serious blood cancers.
Our mission is to ensure every patient has an equal chance to survive and thrive after a stem cell transplant. We take these results extremely seriously, and are calling on urgent action to address the causes of these inequities.
Why do these inequities exist?
While this is the largest study ever in the UK to investigate the impact of ethnicity on stem cell transplant outcomes, there was not enough data to discover the causes of inequities.
Understanding the scale of the issue is an important first step to drive change. Now, this information will help guide our future research to unpick and address the causes of inequities.
Some of the possible causes that require further research are:
- Although the level of tissue type matching between patients and donors was accounted for in this study, there could still be additional genetic differences between patients and donors that affect the outcome of a transplant. Anthony Nolan is currently investigating possible undiscovered genetic markers that could help improve matching in future.
- Genetic variants more common in certain populations could affect how patients respond to treatment or medications. One example is a side effect from transplant called thrombotic microangiopathy (TMA), which can be more severe in people from minority ethnic backgrounds.
- The speed at which patients get to their transplant. We know that it can be harder for patients from minority ethnic backgrounds to find a matching donor, and even though level of matching was controlled for in this study, having a longer wait for a donor could affect patient outcomes.
- Socioeconomic factors that may be involved in inequities. UK census data shows that factors such as housing status, distance from transplant centres, and family income can differ between ethnicities. Factors like these could affect the outcome of a stem cell transplant.
What Anthony Nolan is doing
Anthony Nolan has been researching possible causes of inequities for many years, and is urgently calling for more funding to continue and expand this research.
Our longest-running research project is the Patient/Donor Project, which helps us understand the genetic and clinical factors that make a transplant successful. This project has the potential to reveal new genetic markers that could help address some causes of inequity linked to the way donors are selected for patients. This project has made a huge impact on the world of stem cell transplants in its 20+ year history – including providing the evidence to lower our donor recruitment age to 16. You can read more about the Patient/Donor Project here.
Our SEQoL study (which stands for SocioEconomic and Quality of Life data) aims to evaluate if socioeconomic factors or ethnicity are associated with different healthcare outcomes. The study will help identify areas of transplant care that can be improved to address inequities. You can read more about SEQoL here.
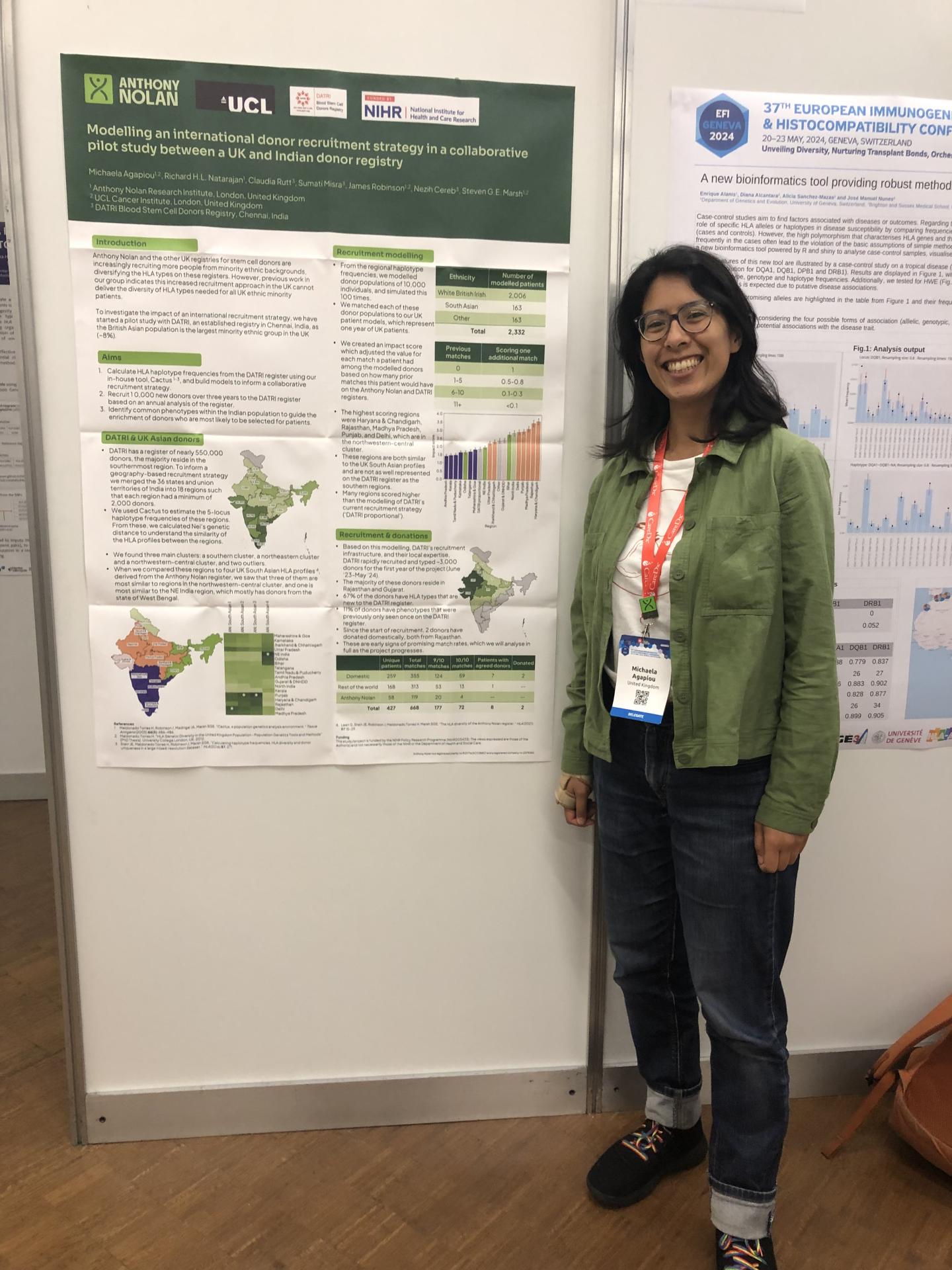
We are collaborating with an Indian stem cell register, DATRI, to investigate new recruitment strategies that could potentially address inequities in donor matching. The project aims to address the global lack of donors with South Asian ancestry, by recruiting from specific areas of India we predict have higher numbers of donors with tissue types most commonly needed for this population. It’s thought that donors with these tissue types will be more likely to be matches for patients with South Asian heritage around the world. You can read more about the DATRI project here.
Our immunotherapy team also researches potential new cell therapies that could reduce the need for a high level of genetic matching between patients and donors, and therefore help level the playing field for patients from minority ethnic backgrounds. Most of our research in this area is focused on the potential of immune cells called natural killer (NK) cells, which have strong anti-cancer capabilities. You can read more about this research here.
We established our Cord Blood Programme in 2008 which has since collected over 50,000 lifesaving umbilical cord blood units, yielding an inventory of nearly 10,000 high quality cords suitable for transplant. These cord blood units can be an important lifeline for patients from minority ethnic backgrounds who might otherwise not find a viable unrelated adult donor.
This is just a glimpse into the work we are doing to improve equity in stem cell transplants. We’re continually developing our understanding of health inequities as part of our aim to realise equitable healthcare and outcomes for every patient.
Advances around the world
Outside our own research, much is being done around the world to try and make stem cell transplants more accessible and successful for all patients.
Of particular note is post-transplant cyclophosphamide (PTCy), which is a treatment given to someone undergoing a stem cell transplant to help reduce the severity of side effects, especially in patients who don’t have a fully matched donor. Cyclophosphamide has been used post-transplant in autologous and haplo-transplants for many years, but emerging research from the US has shown that it can also be given to patients who have had a transplant from an unrelated donor with a slight mismatch to give them the same chance of a positive outcome as patients with a well-matched donor. This could drastically widen the available donor pool for patients with rarer tissue types, so could make a huge impact on healthcare inequities. Several transplant centres in the UK have started using PTCy in specific cases, but there is more work to do to understand its full potential.
Other major work happening across the world includes the development of new cell therapies that can reduce the need for full tissue type matching. Some cell therapies, including CAR-T therapy, involve genetic modification of cells so that they don’t need to be closely matched to the patient’s tissue type. While therapies like these are currently quite expensive or inaccessible, we are campaigning to change government policies and reduce the cost of the development of therapies like these.
There is also much campaigning to improve the representation of people from minority ethnic backgrounds in clinical trials. Currently, clinical trials and large genetic studies are overwhelmingly made up of patients with white European or North American heritage. This leads to a biased view of genetics and means we sometimes don’t know how medicines work for people with genetic variants found more commonly in different parts of the world. In our work with the clinical trials organisation ACT, we are pushing to improve representation in clinical trials in the UK.
What's next?
Anthony Nolan will strive to address healthcare inequities so that everyone, no matter their characteristics, will have fair access to treatments with the best possible outcomes.
While we’re working towards our goals with our research, donor recruitment and partnerships, you can help too. Spread the word about this research and the vital need for more funding. Talk to your MP about the need for more government support to address healthcare inequities. And encourage people to sign up to the Anthony Nolan register to give more patients a chance to find a well-matched donor.
Follow us on our social media channels to stay informed about our progress.
Patient support
Our patient services team can help you if you have any concerns about this new research. You can contact them at patientinfo@anthonynolan.org, or call 0303 303 0303.
Acknowledgements
Anthony Nolan would like to acknowledge the contribution of Dr Richard Szydlo, a senior Medical statistician who contributed to this work. Richard passed away in December 2023 and is remembered by his wife, Blanka, and children Tomek, Robert and Anna.
Full paper reference
Neema P Mayor, Richard M Szydlo, Yasmin Sheikh, Julia Lee, Rachel M Pearce, Caitlin Farrow, Michaela Agapiou, Kanchan Rao, Kim Orchard, Eduardo Olavarria, Steven G E Marsh & John A Snowden.
The impact of patient ethnicity on haematopoietic cell transplantation outcome: a retrospective cohort study on the UK experience,
The Lancet Haematology,
Volume 11, Issue 12,
2024,
Pages e916-e926,
ISSN 2352-3026,
https://doi.org/10.1016/S2352-3026(24)00312-0.